
Can Bronchiolitis cause Asthma in children?
Bronchiolitis and asthma are two common respiratory conditions that often raise concerns and questions among parents and healthcare providers. Understanding the relationship between these two conditions, particularly whether bronchiolitis can lead to asthma, is essential for effective management and prevention strategies. This article explores the possible connections between the two conditions, based on current medical research and clinical observations.

Understanding Bronchiolitis
Bronchiolitis is a respiratory condition primarily affecting infants and young children under two years old. It involves the inflammation of the bronchioles, the small airways in the lungs, usually due to viral infections like the Respiratory Syncytial Virus (RSV). Symptoms include wheezing, coughing, difficulty breathing, and sometimes fever.
What is Asthma?
Asthma is a chronic inflammatory disease of the airways characterized by recurrent episodes of wheezing, breathlessness, chest tightness, and coughing. These symptoms are often related to widespread but variable airflow obstruction within the lung and an increased reaction to various stimuli.
The Connection Between Bronchiolitis and Asthma
Epidemiological Links
Numerous studies have observed a higher incidence of asthma in children who have had severe bronchiolitis in infancy. This observation has led to the hypothesis that there might be a causal link between bronchiolitis and the later development of asthma.
Shared Risk Factors
Both bronchiolitis and asthma share common risk factors, including genetic predisposition, environmental factors like exposure to tobacco smoke, and a history of atopy or allergies.
Immunological and Structural Changes when Bronchiolitis Cause Asthma attacks
Bronchiolitis, especially when severe, can lead to changes in the lung’s structure and immune responses. These changes might predispose an individual to asthma. However, it’s still unclear whether bronchiolitis causes these changes or if they are pre-existing factors that increase the risk for both conditions.
Does Bronchiolitis Cause Asthma?
While there is a notable correlation between bronchiolitis and asthma, it’s important to distinguish correlation from causation. Current research suggests several possibilities:
- Bronchiolitis as a Marker: Bronchiolitis may be an early marker of a pre-existing tendency toward developing asthma, rather than a direct cause.
- Independent but Interrelated: Bronchiolitis and asthma may develop independently of each other but share common risk factors and underlying mechanisms.
- Bronchiolitis as a Trigger: Severe bronchiolitis, particularly when associated with certain viruses like RSV, may trigger the onset of asthma in genetically predisposed individuals.
Clinical Implications and Management
Given the potential link between bronchiolitis and asthma, it’s crucial for parents and healthcare providers to monitor children who have had bronchiolitis for signs of asthma. Preventive measures such as avoiding tobacco smoke exposure, managing allergies, and following recommended vaccinations can be beneficial.
The relationship between bronchiolitis and asthma is complex and multifaceted. While there is an association, more research is needed to fully understand whether bronchiolitis causes asthma or if they are linked through shared risk factors. Ongoing monitoring and preventive strategies are key in managing children at risk.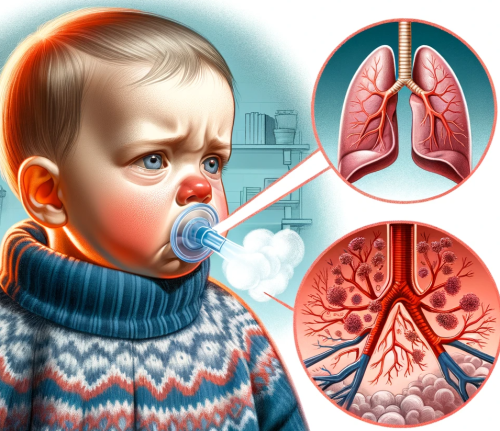
How to prevent bronchiolitis cause asthma?
Preventing the progression of bronchiolitis to asthma, particularly in young children, requires a multifaceted approach focused on reducing exposure to risk factors and enhancing overall respiratory health. Firstly, minimizing exposure to respiratory viruses, especially during infancy, is crucial. This involves practising good hygiene, such as frequent handwashing, and avoiding contact with sick individuals.
Vaccination plays a pivotal role; ensure timely administration of recommended vaccines, including the annual flu shot and, when available, the RSV vaccine. Environmental control is equally important. Reduce exposure to allergens like dust mites, pet dander, and tobacco smoke, as these can aggravate respiratory conditions.
Strengthening the child’s immune system through a balanced diet rich in fruits and vegetables, adequate sleep, and physical activity can also help build resilience against respiratory infections. Breastfeeding for at least six months is advised, as it offers antibodies that protect against various infections. For high-risk infants, such as those born prematurely or with a family history of asthma, prophylactic treatments and close monitoring for early signs of respiratory issues are recommended.
Lastly, managing coexisting conditions like eczema or allergies effectively can reduce the likelihood of developing asthma following bronchiolitis. These preventive measures, combined with regular paediatric check-ups, play a vital role in mitigating the risk of bronchiolitis leading to asthma.
Nutritional Support:
Supplements for Children to Stop Bronchiolitis cause asthma
In managing young children with high risk of the ration “Bronchiolitis Cause Asthma”, and to potentially prevent the progression and long-term development of asthma condition, certain food supplements and vitamins may play a supportive role alongside standard medical treatments. It’s essential to consult with a healthcare provider before starting any supplements, especially in young children. Here are some supplements and vitamins that may be beneficial:
- Vitamin D: Some studies suggest that Vitamin D plays a role in immune function and may help reduce the severity of respiratory infections. Adequate Vitamin D levels might also be protective against asthma development.
- Probiotics: Probiotics, particularly certain strains of Lactobacillus and Bifidobacterium, may help strengthen the immune system. They are thought to positively influence gut health, which is closely linked to immune function.
- Omega-3 Fatty Acids: Found in fish oil, these fatty acids have anti-inflammatory properties that might be beneficial in reducing airway inflammation associated with respiratory conditions.
- Zinc: Known for its immune-boosting properties, zinc may help reduce the duration and severity of respiratory infections. However, it’s important to use it within recommended limits, as excessive zinc can have adverse effects.
- Vitamin C: While the role of Vitamin C in preventing asthma is not entirely clear, it is known for its general immune-boosting properties and may help reduce the duration of colds.
- Antioxidant-rich Foods: While not supplements, diets rich in antioxidants from fruits and vegetables may support lung health and immune function.
- Honey (for children over 1 year): Honey has natural antibacterial properties and may soothe coughs, though it should never be given to children under one year due to the risk of botulism.
Remember, while these supplements and dietary components can support overall health, they are not a substitute for medical treatment. The best approach to managing and preventing bronchiolitis cause asthma, and preventing long-term development of asthma is a combination of a healthy diet, regular medical check-ups, and adherence to any prescribed treatments. Always discuss with a paediatrician before starting any new supplement regimen for a child.
Sports Activities to Prevent and Stop
Bronchiolitis Cause Asthma in Children
Engaging children in regular physical activity is a vital strategy in preventing bronchiolitis cause asthma attacks, and potentially reducing the risk of developing asthma. Sports and physical activities help in strengthening the respiratory system, enhancing lung capacity, and improving overall immune function. Here are some sports activities that can be particularly beneficial:
- Swimming: Often recommended for children with respiratory issues, swimming is an excellent exercise for enhancing lung capacity and control. The humid environment of indoor pools is also generally well-tolerated by those with respiratory sensitivities.
- Cycling: This low-impact exercise can be done outdoors or indoors and is effective in building endurance and respiratory strength without putting excessive strain on the lungs.
- Running and Jogging: These activities, especially when done in a clean, open environment, can significantly improve cardiovascular and pulmonary health. Start with short distances and gradually increase as the child’s endurance builds.
- Team Sports: Participating in team sports like soccer, basketball, or field hockey not only improves physical fitness but also enhances lung function through aerobic exercise.
- Yoga: While not a traditional sport, yoga’s emphasis on controlled breathing can be extremely beneficial for lung health. It teaches children to control their breathing and can help in managing asthma symptoms.
- Outdoor Activities: Activities like hiking, brisk walking, or playing in parks can be beneficial. The exposure to varied environments can help in building a more robust immune system.
It’s important to note that each child’s capabilities and health status are unique, and activities should be chosen to consider their current health condition and in consultation with their healthcare provider. In the case of children with pre-existing respiratory issues, it’s crucial to monitor their response to exercise and adjust accordingly. Regular sports participation, combined with a healthy lifestyle, can play a significant role in preventing bronchiolitis and managing asthma symptoms in children.
Red and Amber Flags for Babies and Children with Bronchiolitis or asthma attack
 In infants and young children, the condition bronchiolitis cause asthma attacks quite often, and can sometimes lead to serious respiratory distress. Parents and caregivers should be vigilant for certain ‘red flags’ that indicate the need for immediate medical attention. These warning signs include:
In infants and young children, the condition bronchiolitis cause asthma attacks quite often, and can sometimes lead to serious respiratory distress. Parents and caregivers should be vigilant for certain ‘red flags’ that indicate the need for immediate medical attention. These warning signs include:
- Reduced Oral Intake: Difficulty or refusal to feed is a significant concern. Infants who cannot take more than half of their usual volume during the last two or three feeds, or those who have not had a wet diaper for 12 hours, may be dehydrated.
- Shortness of Breath: Rapid breathing or difficulty breathing are critical signs. Look for an increased rate of breathing, which for infants is typically more than 60 breaths per minute.
- Intercostal Recessions: Watch for noticeable sucking in between the ribs during inhalation. This is a sign of increased work of breathing.
- Development of Tracheal Tug: This is a sign of severe respiratory distress where the trachea (windpipe) tugs inwards at the neck during breathing efforts.
- Persistent Coughing: A severe or ongoing cough that interferes with feeding or causes vomiting can be a warning sign.
- Lethargy or Irritability: Unusual tiredness, lack of energy, or irritability can indicate a worsening condition.
- Cyanosis: Look for any bluish discoloration around the lips or fingernails, indicating a lack of oxygen.
If any of these symptoms are observed, especially in babies under one year old, it’s crucial to seek medical attention promptly. Early intervention can prevent complications and ensure the best possible outcome for the child.
Bronchiolitis Cause Asthma: A Summary
The intricate relationship between bronchiolitis and asthma is a significant area of interest in pediatric respiratory health. Bronchiolitis, primarily a viral infection of the young child’s lower respiratory tract, has been observed to potentially set the stage for the development of asthma later in life.
So, can bronchiolitis cause asthma actually? Yes, it can, but this connection, however, is complex and multifactorial, and needs further assessment, investigations and all preventative measure taken into consideration when fighting back any of the conditions or the combination of both.
While a direct causal link has not been definitively established, the evidence suggests a strong correlation, particularly in children who experience severe bronchiolitis. The shared risk factors, such as genetic predisposition and environmental triggers, play a crucial role in this association.
Furthermore, the immune responses and structural changes in the lungs due to bronchiolitis may predispose children to asthma. It’s essential to understand that bronchiolitis may not cause asthma per se, but it could be a significant marker or a trigger in genetically susceptible individuals.
The overlapping clinical presentations of both conditions necessitate careful monitoring and management. Acknowledging this potential link guides pediatric care towards more proactive and preventive strategies, aiming to reduce the burden of respiratory illnesses in children and improve long-term respiratory health outcomes.
Where to Seek Help and Stop Bronchiolitis Cause Asthma in Children in the UK, United States and Australia
Bronchiolitis, particularly when it leads to or is associated with asthma, can result in significant complications requiring prompt medical attention. Parents in England, the United States, and Australia should be aware of where to seek help if their child exhibits severe symptoms or complications related to these conditions.
In England, the NHS provides comprehensive pediatric care. In major cities like Manchester, the Royal Manchester Children’s Hospital, equipped with an A&E department, offers specialized pediatric emergency medicine. Similarly, in London, the Great Ormond Street Hospital is renowned for its pediatric expertise. For non-emergency situations, local GP practices and NHS 111 can offer guidance and referrals.
In the United States, children’s hospitals are located in most major cities and provide specialized pediatric care. For instance, the Children’s Hospital of Philadelphia and Boston Children’s Hospital are among the top facilities for pediatric respiratory issues. Parents can also seek help at local hospitals’ emergency departments or consult their pediatrician for advice and referrals.
Australia boasts several excellent pediatric facilities. The Royal Children’s Hospital in Melbourne and the Sydney Children’s Hospital in Randwick are notable examples, providing comprehensive care for various pediatric health concerns, including respiratory issues like bronchiolitis and asthma.
Parents should not hesitate to seek emergency care in the event of severe respiratory distress, persistent coughing, difficulty breathing, or any signs of cyanosis (bluish discoloration of the skin). For less urgent concerns, scheduling a visit with a pediatrician or a local GP for ongoing management and advice is advisable. Remember, timely medical intervention can prevent complications and ensure the best possible outcome for the child’s health.
- Fish Oil – 7 Major Benefits For Great Mood
- 5 Essential Facts in Our Master Guide to Adenoids or Third Tonsil
- ADHD in Children: Identify and 10+ Ways to Master the Symptoms
- How to Treat Constipation Effectively? 10+ Amazing to-do Strategies
- Can Bronchiolitis Cause Vomiting and Why? 4 Master Reasons
Article by Dr Tsanko Stefanov

